Understanding the Critical Role of the Inner Ear in Maintaining Balance
The inner ear is an extraordinary anatomical structure that serves as a key player in sustaining balance through the sophisticated mechanisms of the science behind ear balance. Central to this process is the vestibular system, which is intricately designed to detect motion and uphold equilibrium. This system is essential for our daily activities, allowing us to perceive and respond to our surroundings without losing our footing. Its remarkable sensitivity to environmental changes empowers us to navigate various terrains, thereby enhancing our overall mobility and safety.
Comprehensive Overview of the Vestibular System’s Functionality

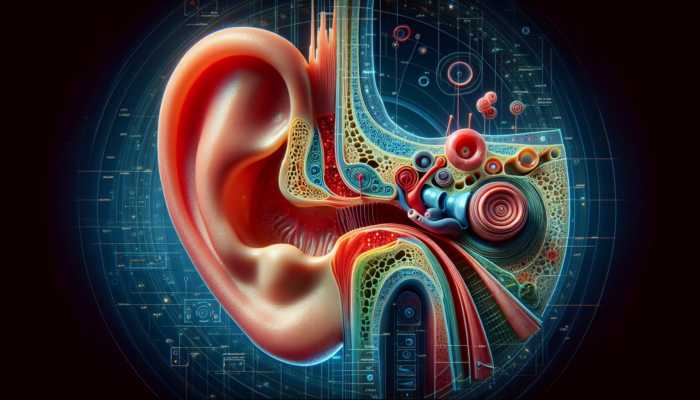
The vestibular system is fundamentally accountable for our sense of balance. Situated within the inner ear, it encompasses three semicircular canals filled with fluid and two otolith organs. As we move through space, the fluid within these canals shifts, stimulating sensory hair cells that transmit signals to the brain. This critical process informs the brain about our spatial positioning and motion, enabling us to maintain stability whether we are walking, running, or standing still. The intricate design of this system showcases how our body seamlessly adapts to various forms of movement.
Moreover, the vestibular system does not operate in isolation; it collaborates closely with our visual system and proprioceptive system. This integration is essential for achieving a thorough understanding of our body’s orientation in three-dimensional space. For example, when we turn our heads, the vestibular system detects this positional change while our eyes provide visual feedback, and proprioceptors in our muscles and joints relay information about body position. This synergy is paramount for activities requiring coordination and spatial awareness, such as sports, dance, or even navigating uneven surfaces.
Various factors can influence the functionality of the vestibular system. Changes associated with aging, inner ear infections, or physical injuries can compromise its effectiveness, leading to balance disruptions. Understanding the role of the vestibular system is crucial for formulating strategies aimed at enhancing balance and preventing falls, particularly in populations that are more vulnerable, such as the elderly. By focusing on these aspects, we can foster greater awareness of balance health and its implications for overall well-being.
Understanding the Essential Functions of Semicircular Canals
The semicircular canals are among the most vital components of the vestibular system. Each canal is uniquely positioned at a different angle, enabling them to detect rotational movements across all axes—up, down, left, right, and diagonal. As we rotate our heads, the fluid within these canals moves and bends the hair cells, which send precise signals to the brain that inform us about our rotational movements. This mechanism is crucial for maintaining our sense of balance and ensuring smooth coordination during various physical activities.
This functionality is not only essential for balance; it also significantly contributes to our coordination during movements. For instance, athletes heavily rely on their semicircular canals to adjust their movements swiftly in response to rapid changes in direction or speed. Similarly, dancers depend on this system to execute precise turns without compromising their stability, while pilots utilize it to maintain their orientation during complex flight maneuvers. The ability to accurately sense rotational changes is paramount for effective performance in any physical discipline.
Gaining insight into the functioning of the semicircular canals can help highlight potential balance-related issues. Conditions such as vestibular neuritis or benign paroxysmal positional vertigo (BPPV) can interfere with the normal operation of these canals, leading to symptoms like vertigo or dizziness. Recognizing these conditions is the first step towards addressing balance disorders and implementing effective treatment strategies that can restore normal function and improve quality of life.
Otolith Organs: The Key to Understanding Gravity and Linear Movement
The otolith organs, which consist of the utricle and saccule, work in conjunction with the semicircular canals to detect linear acceleration and the force of gravity. These organs contain microscopic crystals known as otoliths, which shift in response to variations in head position or movement. This shifting action stimulates hair cells and sends signals to the brain about the body’s orientation concerning gravity, providing critical information necessary for maintaining balance.
The importance of the otolith organs extends far beyond simple balance maintenance. They play a pivotal role in our spatial awareness, enabling us to perceive our position in relation to the ground. For instance, when we lean forward, the otoliths shift, relaying essential information to the brain to adjust our posture and maintain stability. This dynamic feedback loop is vital for everyday activities, ensuring we can interact confidently with our environment.
The function of these organs becomes particularly crucial during activities that demand acute spatial awareness, such as mountain climbing or maneuvering through crowded spaces. The ability to perceive gravity and linear movement aids individuals in maintaining their footing and avoiding obstacles, which is essential for safety across various contexts. Understanding the role of the otolith organs can also illuminate common balance disorders, as disruptions in their function can lead to conditions like BPPV, resulting in sudden and debilitating dizziness.
Exploring the Neurological Pathways that Facilitate Balance

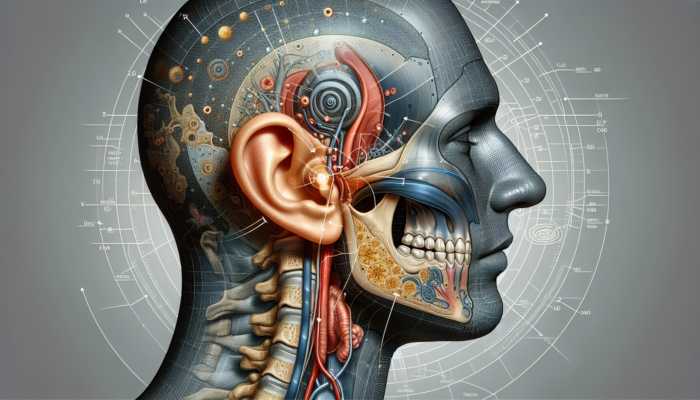
Balance is a complex phenomenon that is not solely reliant on the inner ear; it is intricately connected to a network of neurological pathways that transmit and process sensory information. The vestibular nerve serves as a crucial conduit, relaying balance information from the inner ear to the brain. This intricate interplay between the vestibular system and various brain regions is vital for maintaining coordination and stability during movement.
Transmission of Balance Information Through the Vestibular Nerve
The vestibular nerve acts as the primary pathway for transmitting balance information from the inner ear to the brain, primarily targeting the vestibular nuclei located in the brainstem. This transmission process is essential for coordinating the motor responses that keep us upright and stable. As the vestibular nerve communicates with the brain, it conveys information not only about head movements but also about our body’s position in three-dimensional space.
When we engage in movement, the vestibular nerve generates electrical impulses that relay information to various brain regions, including the cerebellum and the spinal cord. This communication is crucial for real-time adjustments to muscle activity and posture. For instance, if we begin to lose our balance while walking, the vestibular nerve sends corrective signals that prompt our muscles to engage and stabilize our stance. This ongoing feedback mechanism is vital for seamless movement and overall stability.
Research indicates that the efficiency of vestibular nerve transmission can significantly impact our balance capabilities. Factors such as aging, neurological disorders, or vestibular dysfunction can impair this transmission, leading to balance issues. Understanding how the vestibular nerve operates is crucial for developing effective interventions for individuals experiencing balance disorders, ensuring they receive the necessary support to regain their stability and independence.
The Integral Roles of the Brainstem and Cerebellum in Balance
The brainstem and cerebellum play vital roles in processing vestibular inputs and coordinating balance responses. The brainstem integrates sensory information from the vestibular system, visual system, and proprioceptive system to create a comprehensive understanding of our body’s position and movement in space. This integration is crucial for maintaining equilibrium during dynamic activities.
The cerebellum, often referred to as the brain’s coordination center, is instrumental in fine-tuning motor responses based on the information received from the vestibular nerve. By processing data rapidly, the cerebellum can initiate appropriate muscle adjustments, aiding in balance maintenance during dynamic movements. For athletes, dancers, and individuals engaged in physical activities, the seamless collaboration of these brain regions ensures optimal performance and safety.
Disruptions in the functioning of the brainstem or cerebellum can lead to balance disorders. Conditions such as cerebellar ataxia or multiple sclerosis can impair the brain’s ability to process vestibular information, resulting in significant challenges in maintaining equilibrium. Recognizing the roles of these brain regions in balance can inform treatment strategies and rehabilitation efforts for those affected by balance disorders, enhancing their quality of life and functional capabilities.
The Interplay Between Visual and Proprioceptive Systems in Balance

Balance is a multifaceted process that relies on the integration of information from the vestibular, visual, and proprioceptive systems. This complex interplay enables the brain to construct an accurate representation of our body in space, ensuring we can move confidently and safely through our environment. The visual system provides contextual awareness about our surroundings, allowing us to identify obstacles and changes in terrain.
When we navigate through dynamic environments, such as a crowded market or a hiking trail, our eyes gather vital information that complements the data provided by the vestibular system. This integration is crucial for preventing falls and maintaining stability, particularly in settings where the ground may be uneven or unpredictable. The ability to process this multifaceted information is what allows us to move with grace and confidence.
Proprioception, which refers to the body’s ability to sense its position and movement, adds another layer of depth to the balance equation. Proprioceptors located in our muscles and joints relay critical information about body posture and movement, enabling the brain to make real-time adjustments. For example, if we step onto an uneven surface, proprioceptors send signals to the brain, prompting immediate muscle adjustments to maintain balance. This feedback loop is vital for daily activities and overall safety.
Understanding the intricate connections among these systems is essential for addressing balance disorders. Rehabilitation strategies that focus on enhancing visual and proprioceptive input alongside vestibular training can significantly improve balance and stability. By fostering collaboration among these systems, individuals can reclaim their confidence and independence in daily activities, ultimately leading to a better quality of life.
Identifying Common Balance Disorders and Their Implications
Despite the sophisticated mechanisms governing balance, various disorders can disrupt these processes, leading to symptoms such as dizziness, vertigo, and instability. Gaining a comprehensive understanding of these common balance disorders is crucial for effective diagnosis and treatment, allowing for timely interventions and improved outcomes.
Understanding Vestibular Neuritis and Its Impact
Vestibular neuritis is a disorder characterized by inflammation of the vestibular nerve, often linked to viral infections. The sudden onset of vertigo—a profoundly disorienting spinning sensation—can be debilitating. Individuals affected by this condition may struggle to walk or concentrate on daily tasks, significantly affecting their quality of life. The intense nature of the symptoms can lead to heightened anxiety and frustration.
Symptoms of vestibular neuritis typically manifest abruptly, frequently following a respiratory infection. Individuals experience prolonged episodes of vertigo, which can last for several days. Accompanying symptoms may include nausea, imbalance, and visual disturbances. Understanding the triggers and symptoms associated with vestibular neuritis is vital for prompt recognition and management, ensuring individuals receive the appropriate care to alleviate their symptoms.
Treatment for vestibular neuritis often consists of a combination of medications aimed at alleviating symptoms and vestibular rehabilitation therapy (VRT) to facilitate recovery. VRT incorporates exercises designed to help individuals adapt to changes within their vestibular system, ultimately improving balance and reducing the risk of future episodes. With appropriate intervention, individuals can regain their balance and confidence in their daily activities, leading to enhanced overall well-being.
Benign Paroxysmal Positional Vertigo (BPPV): Causes and Treatments
Benign paroxysmal positional vertigo (BPPV) is a common balance disorder caused by dislodged crystals in the inner ear. These crystals, known as otoconia, can shift into the semicircular canals, resulting in brief episodes of dizziness triggered by specific head movements. Activities such as rolling over in bed or looking up can provoke intense sensations of spinning, which can be both alarming and disruptive to daily life.
Symptoms of BPPV tend to be brief, usually lasting less than a minute, but their frequent occurrence can lead to significant anxiety regarding the unpredictable nature of the symptoms, adversely affecting daily routines. Understanding the mechanics of BPPV is crucial for individuals experiencing these symptoms, as this knowledge empowers them to seek appropriate treatment and manage their conditions effectively.
Treatment options for BPPV typically include a series of repositioning maneuvers designed to guide the dislodged crystals back to their correct location within the inner ear. These maneuvers, such as the Epley maneuver, can provide rapid relief and restore balance. In addition, educating individuals on symptom management can enhance their ability to navigate daily activities with greater confidence and less fear of triggering episodes.
Ménière’s Disease: Understanding a Chronic Inner Ear Disorder
Ménière’s disease is a chronic inner ear condition characterized by fluid accumulation, leading to episodes of vertigo, hearing loss, and tinnitus (ringing in the ears). The unpredictable nature of these episodes can significantly impact an individual’s quality of life, leading to feelings of anxiety and frustration. Individuals may experience sudden and severe vertigo attacks that can last from minutes to hours, often accompanied by a sensation of fullness in the ear.
The exact cause of Ménière’s disease remains unclear; however, it is believed to involve an imbalance in fluid regulation within the inner ear. This disorder can make engaging in daily activities challenging, necessitating a comprehensive understanding of its symptoms and management options. Recognizing the signs of Ménière’s disease is essential for individuals seeking timely intervention and support.
Treatment for Ménière’s disease generally involves a combination of dietary modifications, medications, and lifestyle adjustments. Reducing salt intake can help manage fluid levels in the inner ear, while medications can alleviate symptoms during acute episodes. In severe cases, surgical options may be considered to address chronic symptoms. By understanding the intricacies of Ménière’s disease, individuals can collaborate with healthcare professionals to develop effective management strategies that enhance their quality of life.
Diagnostic Techniques for Identifying Balance Issues
Diagnosing balance disorders is a crucial step in formulating effective treatment strategies. A range of diagnostic techniques can assist healthcare professionals in assessing the underlying causes of balance issues, ensuring accurate identification and management of various conditions. Employing these techniques can facilitate timely intervention, ultimately improving patient outcomes.
Electronystagmography: Evaluating Vestibular Function
Electronystagmography (ENG) is a diagnostic test designed to measure eye movements to evaluate vestibular function. By tracking the way the eyes respond to various stimuli, clinicians can obtain valuable insights into the health of the vestibular system. During the test, electrodes are placed around the eyes to record movements while the patient is subjected to specific head and body positions.
ENG is particularly effective for identifying conditions such as vestibular neuritis or BPPV, as it can reveal abnormalities in the vestibular pathways. The information gathered during the test helps healthcare professionals understand the nature and extent of balance disorders, guiding subsequent treatment decisions to improve patient care.
For individuals experiencing dizziness or balance-related difficulties, ENG can be an invaluable tool for uncovering underlying causes, leading to targeted interventions. By thoroughly assessing the functionality of the vestibular system, clinicians can devise tailored rehabilitation plans aimed at enhancing balance and alleviating symptoms.
Vestibular Evoked Myogenic Potentials: Assessing Otolith Function
Vestibular evoked myogenic potentials (VEMP) testing serves as another diagnostic tool that evaluates the function of the otolith organs. By measuring muscle responses in the neck or eyes to sound stimuli, clinicians can assess the integrity of the vestibular pathways. This test is particularly useful for identifying dysfunctions related to the otolith organs, which can contribute to balance disorders.
During VEMP testing, sound stimuli are delivered through headphones while electrodes monitor muscle responses. By analyzing the data collected, healthcare professionals can determine how effectively the otolith organs are functioning and their role in maintaining balance. This diagnostic tool can reveal critical insights into the underlying causes of balance issues, paving the way for appropriate treatment strategies.
Understanding the function of the otolith organs is essential for diagnosing conditions such as BPPV or Ménière’s disease. Utilizing VEMP testing allows clinicians to gain a deeper understanding of a patient’s vestibular health, enabling them to design effective treatment strategies that specifically address balance challenges.
Rotational Chair Testing: A Comprehensive Assessment of Vestibular Function
Rotational chair testing is a thorough assessment that evaluates the vestibular system‘s response to rotational movements. During this test, the patient is seated in a specialized chair that rotates at controlled speeds while eye movements are closely monitored. This assessment provides valuable insights into the functionality of the vestibular system and its ability to process dynamic information.
This testing method can help identify vestibular disorders by assessing how well the system adapts to changes in motion. By analyzing eye movements throughout the test, clinicians can detect abnormalities in the vestibular pathways, thereby guiding treatment plans for individuals experiencing balance challenges. The results can inform rehabilitation strategies tailored to individual needs.
For individuals dealing with persistent dizziness or instability, rotational chair testing can be an essential diagnostic tool. By grasping the intricacies of vestibular function, healthcare professionals can develop targeted rehabilitation strategies aimed at improving balance and enhancing overall well-being.
Effective Treatment Approaches for Balance Disorders
When addressing balance disorders, a variety of treatment approaches are available to help individuals regain their stability and confidence. From rehabilitation exercises to medication management, understanding the array of options is crucial for effective intervention and successful management of symptoms.
Vestibular Rehabilitation Therapy: Enhancing Balance Through Targeted Exercises
Vestibular rehabilitation therapy (VRT) is a specialized form of physical therapy designed to improve balance and reduce dizziness. This therapeutic approach involves a series of targeted exercises aimed at retraining the vestibular system, helping individuals adapt to changes in their balance mechanisms. VRT is particularly beneficial for those with vestibular disorders, as it focuses on enhancing the brain’s ability to process vestibular information effectively.
During VRT, individuals participate in exercises that promote balance and stability, often incorporating movements that challenge their vestibular responses. These workouts may include head movements, gaze stabilization techniques, and balance training exercises that gradually increase in complexity. The primary goal is to improve the brain’s capacity to interpret sensory information accurately, ultimately reducing dizziness and enhancing overall balance.
Research supports the efficacy of VRT in improving balance outcomes, especially for individuals with conditions like vestibular neuritis or BPPV. By fostering a proactive approach to balance recovery, VRT empowers individuals to take control of their symptoms, regain confidence in their daily activities, and improve their quality of life.
Medications for Symptom Management in Balance Disorders
Medications can significantly contribute to managing the symptoms associated with balance disorders. A wide range of pharmaceutical options is available to alleviate symptoms such as dizziness, nausea, and vertigo, providing individuals with relief during acute episodes. Common medications include antihistamines, antiemetics, and vestibular suppressants.
Antihistamines, such as meclizine, are effective in reducing dizziness and nausea associated with vestibular disorders. Anti-nausea medications may also be prescribed to help manage symptoms that arise during vertigo episodes. Additionally, vestibular suppressants can stabilize the vestibular system and provide immediate relief from debilitating symptoms.
While medications can be beneficial, they are often intended as temporary solutions and should be used in conjunction with other therapeutic approaches, such as VRT. Understanding the role of medications in managing balance disorder symptoms empowers individuals to collaborate with healthcare professionals to develop comprehensive treatment plans tailored to their specific needs.
Exploring Surgical Interventions for Severe Balance Disorders
In severe cases where balance disorders significantly impact quality of life, surgical interventions may be considered. Procedures such as labyrinthectomy or vestibular nerve section can provide relief for individuals with chronic balance issues that do not respond to conservative treatments. These surgical options are typically reserved for cases where other therapies have proven ineffective.
Labyrinthectomy involves the removal of a portion of the inner ear responsible for balance, effectively eliminating vertigo symptoms. In contrast, vestibular nerve section entails cutting the vestibular nerve to prevent signals from transmitting to the brain, alleviating debilitating dizziness.
While surgical options can effectively address balance disorders, they come with inherent risks and potential side effects. Individuals considering surgical interventions should engage in comprehensive discussions with healthcare professionals to weigh the benefits against the risks, ensuring informed decision-making that prioritizes their health and well-being.
Implementing Dietary and Lifestyle Modifications for Balance Management
Dietary and lifestyle modifications can significantly influence the management of balance disorders. Simple adjustments, such as reducing salt intake, can help regulate fluid levels in the inner ear, particularly for individuals with Ménière’s disease. Maintaining a balanced diet rich in nutrients that support vestibular health can also contribute positively to overall well-being.
In addition to dietary changes, individuals are encouraged to adopt a healthy lifestyle that incorporates regular physical activity. Engaging in exercises that promote strength and balance can enhance stability, thereby reducing the risk of falls. Activities such as yoga, tai chi, and strength training are particularly effective for improving core strength and maintaining balance.
Furthermore, avoiding triggers like caffeine and alcohol can help manage symptoms for those with vestibular disorders. By recognizing the impact of dietary and lifestyle choices on balance, individuals can take proactive steps to enhance their vestibular health and overall quality of life, ensuring a safer and more stable daily experience.
Addressing Psychological and Cognitive Aspects of Balance Disorders
Psychological and cognitive therapies can be immensely valuable in addressing the emotional and psychological dimensions of balance disorders. Many individuals experience heightened anxiety and fear related to their symptoms, which can exacerbate feelings of instability and hinder recovery. Cognitive-behavioral therapy (CBT) is an effective approach that helps individuals develop coping strategies and resilience in the face of balance challenges.
CBT focuses on identifying negative thought patterns and replacing them with positive, empowering beliefs. By addressing the psychological impact of balance disorders, individuals can enhance their overall well-being and reduce the anxiety that often accompanies dizziness and instability. Additionally, mindfulness and relaxation techniques can complement therapy, promoting stress management and improving overall quality of life.
Recognizing the significance of psychological support in managing balance disorders paves the way for a holistic treatment approach. By integrating cognitive therapies into their care plans, individuals can foster resilience and regain confidence in their ability to navigate daily life with improved stability.
Proactive Measures for Maintaining Balance and Preventing Disorders
Taking proactive measures to maintain balance is essential for significantly reducing the risk of falls and related injuries. Engaging in preventive strategies is crucial for individuals of all ages, particularly those with a history of balance issues. By focusing on health promotion and awareness, individuals can enhance their quality of life and well-being.
The Importance of Regular Physical Activity for Balance Maintenance
Engaging in regular physical activity stands out as one of the most effective methods for maintaining balance and preventing issues related to instability. Exercises that focus on balance, strength, and flexibility are especially beneficial. Activities such as yoga, tai chi, and dancing not only enhance physical fitness but also foster improved coordination and body awareness.
Incorporating balance training into daily routines can yield profound effects on overall stability. Simple exercises, such as standing on one foot, practicing heel-to-toe walking, or using balance boards, can strengthen stabilizing muscles and improve proprioception. For older adults, participating in group classes or community programs that emphasize balance can provide both social support and enhanced physical capabilities.
Moreover, consistency is key. Engaging in regular exercise routines helps the body adapt and strengthen over time, leading to improved balance and reduced fall risk. Understanding the importance of physical activity in maintaining balance empowers individuals to take charge of their health and well-being, fostering a proactive approach to balance management.
Maintaining Proper Hydration and Nutrition for Vestibular Health
Ensuring adequate hydration and proper nutrition is fundamental for overall health, including maintaining vestibular health. Dehydration can exacerbate symptoms of dizziness and instability, making it crucial to drink sufficient fluids throughout the day. A well-balanced diet rich in vitamins and minerals supports optimal bodily function, including the health of the vestibular system.
Focusing on nutrient-dense foods, such as fruits, vegetables, whole grains, and lean proteins, provides the essential nutrients needed for overall well-being. Omega-3 fatty acids, found in fish and nuts, are particularly beneficial for brain health and may support vestibular function. Ensuring adequate nutrient intake can foster a robust system that supports balance.
Additionally, certain dietary modifications, such as reducing caffeine and salt intake, can help manage symptoms for individuals with vestibular disorders. By prioritizing nutrition and hydration, individuals can create an environment conducive to maintaining balance and overall wellness, leading to enhanced quality of life.
Scheduling Regular Health Check-ups for Early Detection
Regular health check-ups are vital for monitoring overall health and addressing potential balance issues at an early stage. Routine examinations allow healthcare professionals to assess vestibular health, identify any emerging issues, and provide timely interventions that can prevent further complications.
For individuals with a history of balance disorders, regular assessments can help track progress and modify treatment plans as necessary. Additionally, engaging in preventative screenings can help identify underlying conditions that may contribute to balance issues, such as cardiovascular health or vision changes. This proactive approach ensures that any potential problems are addressed promptly, minimizing their impact on daily life.
Early detection and intervention can significantly enhance outcomes, empowering individuals to manage their balance effectively. By prioritizing regular health check-ups, individuals can take proactive steps to safeguard their stability and quality of life, leading to a more confident and secure existence.
Frequently Asked Questions About Balance Disorders
What is the vestibular system and its importance?
The vestibular system, located in the inner ear, is vital for maintaining balance by detecting motion and spatial orientation. It comprises semicircular canals and otolith organs that collaboratively provide information about head position and movement, ensuring stability during various activities.
How does the inner ear influence balance?
The inner ear plays a crucial role in balance through the vestibular system. It detects motion and gravitational forces, relaying signals to the brain that aid in coordinating movements and maintaining stability during different activities.
What are the common symptoms associated with balance disorders?
Common symptoms include dizziness, vertigo, unsteadiness, and difficulty concentrating. These symptoms can vary in severity and significantly impact daily activities and overall quality of life, necessitating timely intervention and management.
How is vestibular neuritis diagnosed and managed?
Vestibular neuritis is diagnosed through a combination of clinical history and diagnostic tests, such as electronystagmography (ENG) or vestibular evoked myogenic potentials (VEMP), which assess vestibular function. Management typically involves medications for symptom relief and vestibular rehabilitation therapy (VRT) to facilitate recovery.
What treatments are available for managing balance disorders?
Treatment options encompass vestibular rehabilitation therapy (VRT), medications for symptom management, lifestyle modifications, and, in some cases, surgical interventions. A personalized approach is essential for effective management and improved patient outcomes.
Can balance disorders be prevented through lifestyle changes?
While not all balance disorders are preventable, engaging in regular physical activity, maintaining proper hydration and nutrition, and scheduling routine health check-ups can significantly reduce the risk of balance-related issues and enhance overall stability.
What role does the cerebellum play in balance regulation?
The cerebellum processes sensory information from the vestibular system and coordinates motor responses, aiding the body in maintaining balance and stability during movement. Its role is crucial for seamless coordination.
How can psychological therapies aid in managing balance disorders?
Psychological therapies, such as cognitive-behavioral therapy (CBT), can assist individuals in coping with anxiety related to balance disorders, empowering them to manage their symptoms effectively and improve overall well-being through enhanced coping strategies.
What is BPPV and its treatment options?
Benign paroxysmal positional vertigo (BPPV) is a condition caused by dislodged crystals in the inner ear, leading to brief episodes of dizziness. Treatment often involves repositioning maneuvers designed to restore balance by guiding the dislodged crystals back to their correct location.
Are there any dietary changes that support balance disorder management?
Yes, dietary changes such as reducing salt intake, avoiding caffeine, and maintaining a balanced diet rich in essential nutrients can support overall vestibular health and help manage symptoms associated with balance disorders.
Discover more on our platform on X!
The post Ear Balance: Understanding the Science Behind It All appeared first on The Microsuction Ear Wax Removal Network.